When "Stopping Your Ozempic" Becomes the Most Expensive Health Decision You'll Make
You hit your goal weight. The medication worked. Then you stopped—maybe your insurance changed, maybe you thought you were done, maybe $200 a month felt like too much once the scale said what you wanted it to say. Now it’s six months later, and the number’s climbing back. And you’re wondering if you imagined the whole thing.
You didn’t imagine it. And you’re not failing.
Here’s the part nobody says out loud when they prescribe weight loss medication: stopping it almost always leads to weight regain.
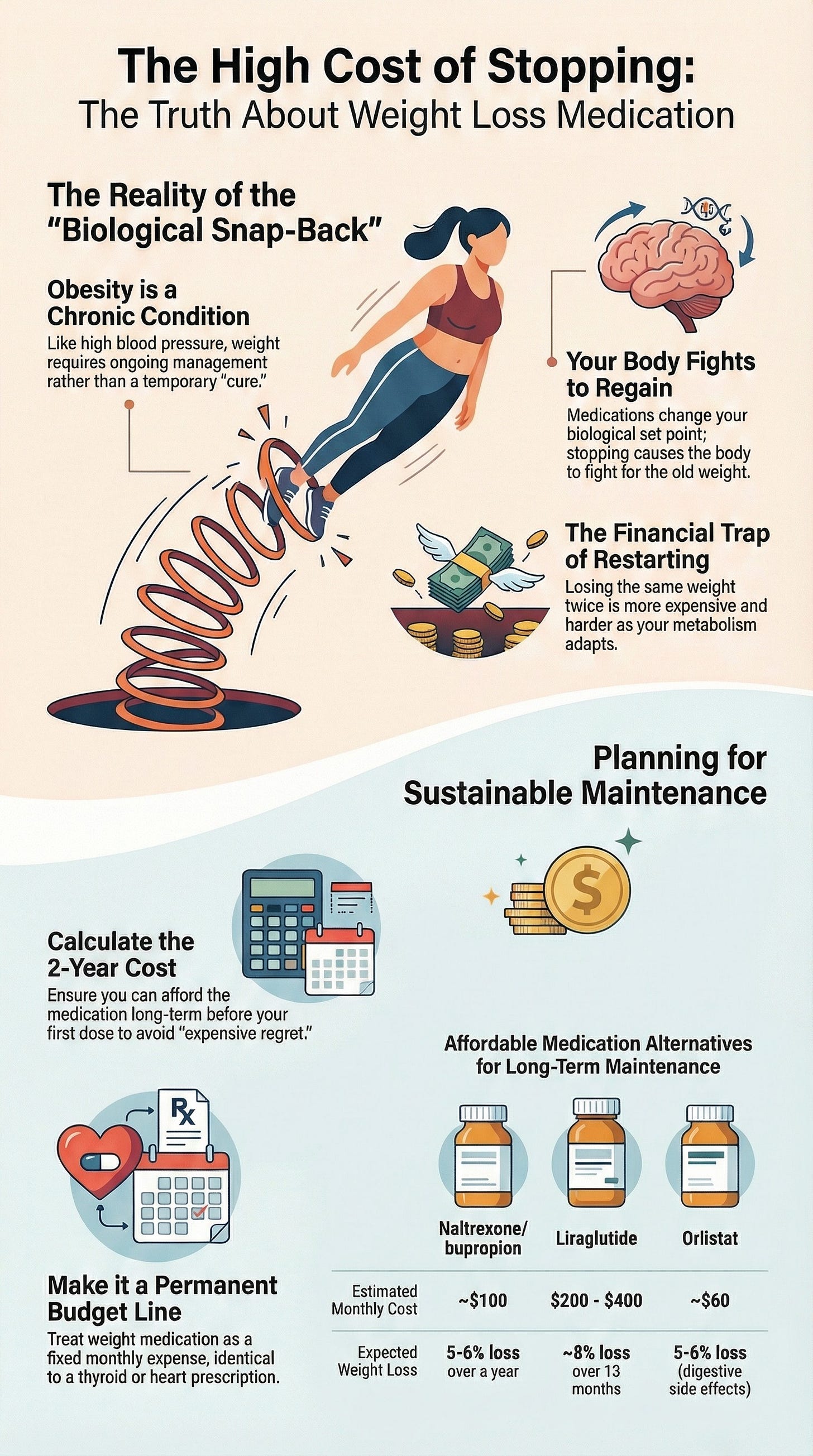
Not because you lack discipline. Because obesity is a chronic condition, and these medications work by changing your body’s biological set point. When you stop, your body doesn’t stay at the new weight—it fights to get back to the old one.
The myth: “Once I lose the weight, I’m done.”
The reality: You’re not treating a temporary problem. You’re managing a long-term condition.
Think about it this way: if you have high blood pressure and medication brings it down, stopping the medication doesn’t mean your blood pressure stays low. It goes back up. Weight works the same way. Research shows that when people stop medications like semaglutide or tirzepatide, most regain significant weight. Your body isn’t broken—it’s responding exactly how biology works.
Here’s the financial trap: You’ve already spent the money to lose the weight. Now you’re watching that investment disappear. And if you decide to restart? You’re paying again to get back to where you already were. The second round is harder—and potentially more expensive—because your metabolism has adapted.
Here’s what this costs you:
Every month of weight regain isn’t just about the scale. It’s the return of symptoms that were affecting your work—the brain fog, the joint pain, the sleep disruption, the energy crashes. It’s the return of health risks that will cost more to treat later. And it’s the psychological cost of feeling like you failed when the real failure was in how the medication was presented to you in the first place.
What To Do Next:
Before you start any weight loss medication, calculate the two-year cost. Not the monthly cost—the actual total. If you can’t afford it long-term, you’re setting yourself up for expensive regret. This isn’t pessimism. It’s protection.
If you’re already in weight regain after stopping, here are the options you can actually afford long-term:
Naltrexone/bupropion - Around $100/month. Delivers 5-6% weight loss over a year. Not dramatic, but steady and sustainable on most budgets.
Liraglutide - Daily injection instead of weekly. About 8% weight loss over 13 months. Often runs $200-400/month depending on insurance, but some manufacturer programs bring it lower.
Orlistat - Available over-the-counter at $60/month or prescription strength. About 5-6% weight loss. Fair warning: the side effects (digestive issues) make this one hard to stick with, which is why doctors don’t reach for it first.
The right choice isn’t the one with the biggest number. It’s the one you can afford to stay on. Talk to your doctor about what works with your budget and your body.
Add “weight medication” as a permanent line item in your budget, not a temporary expense. This is maintenance, not a cure. File it next to your blood pressure medication or your thyroid prescription—because that’s what it is.
You deserve to know the truth before you start.
Reply with one word: RESTARTING or DECIDING.
Forward this to someone who’s been saying, “The medicine didn’t work.”